In Canada, low-income hospital patients under palliative care are less likely to receive medical assistance in dying compared to those who are high income, according to a study published in British Medical Journal Open (BMJ Open).
Medical assistance in dying (MAID) is legal and free under Medicare, Canada’s universal health care system. Patients with low socioeconomic status (SES), however, generally tend to experience less access to medical care compared to their high SES counterparts.

Eldar Shafir, professor of psychology and public affairs at the Princeton School of Public and International Affairs, along with a team of researchers from Sunnybrook Hospital in Ontario, investigated whether this trend of decreased care for low-income patients includes medical assistance in dying.
“I have long been interested in SES influences on decision-making,” said Shafir. “I often discuss with my friend and collaborator, Dr. Redelmeier, ways to illustrate some of our findings in the medical realm, especially, when possible, among experts. … In this case MAID was a really interesting domain, since it’s a ‘big’ decision, and finances are not an issue.”
Medical assistance in dying was ruled legal in Canada in February 2015 and officially implemented and covered under Medicare by June 2016. To be considered, a patient must have a grievous and irremediable medical condition, such as metastatic cancer, that causes unbearable suffering where death is foreseeable, according to the Government of Canada.
However, one’s socioeconomic status can influence how medical care is administered and received by a patient in several ways. “People can be easily susceptible to pitfalls and biases in reasoning,” Shafir said.
Low-income patients, for example, may feel less equipped to advocate for their care and to convey dissatisfaction. Clinicians can also succumb to the “thick-skin fallacy,” or the harmful perception that low-income people are used to hardship and therefore less impacted by it.
The team explored the association between socioeconomic status and medical assistance in dying by identifying hospital patients aged 65 and older in Ontario, Canada between June 2016 and 2019. At the time of their death, all patients, all of whom had serious medical conditions, were under palliative care, receiving pain-relieving treatment for symptoms. They were then divided into groups based on socioeconomic status, which was calculated using an official algorithm created by Statistics Canada based on home neighborhood location, and whether they received medical assistance in dying.
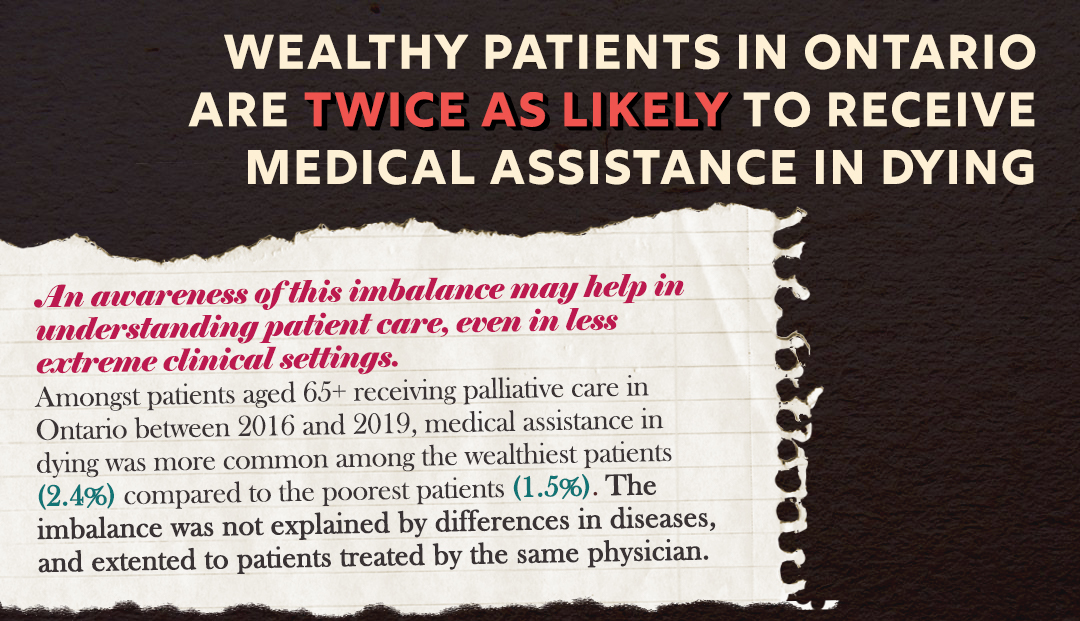
During the three years, 50,096 patients were given palliative care in their last month of life. Among them, 920 received medical assistance in dying. Only 1.5% of low-income patients identified were given MAID, compared to 2.4% of high-income patients — a 39% decreased likelihood for those with low socioeconomic status. This disparity in care was found consistently across a variety of patient subgroups that varied in age, sex, home location, type of cancer, health care utilization, and general frailty. It was even replicated with patients treated by the same responsible physician.
The study’s results support past findings by other countries about the relationship between medical assistance in dying and patients’ socioeconomic status. In countries like the United States, the Netherlands, Switzerland, and Belgium, people who received MAID or MAID equivalents tended to be highly educated, financially secure, or live in wealthy neighborhoods.
The researchers, however, suspect that this difference in patient care may be influenced by factors that exist outside of financial capabilities. “I suspect most of what happens here is a function of the doctor-patient interaction," Shafir said. “I think, all else equal, that doctors might see low-SES patients as less in urgent need of MAID.”
Certain study limitations, such as biased and imperfect socioeconomic status measures, warrant further research exploring the link between social class and medically assisted death. “Both perspectives, the doctors' and the patients', need to be better understood by the medical community in order to provide low-SES patients with same care afforded those of higher SES,” Shafir said.
The observations made by Shafir and his team address an earlier misconception in Canada that medical assistance in dying may harmfully target low-income individuals. The researchers are optimistic that their findings may help promote greater patient-clinician communication and engagement.
“Association of socioeconomic status with medical assistance in dying: a case-control analysis” by Donald A. Redelmeier, Kevin Ng, Deva Thiruchelvam, and Shafir, was published on April 30 in British Medical Journal Open.

